Gallbladder Problems After Bariatric Surgery: Treatment & Prevention
Gallbladder Problems After Bariatric Surgery
Rapid weight loss is one of the most powerful benefits of bariatric surgery—but it also increases the risk of gallstone formation. Many patients ask what happens if the gallbladder becomes an issue after weight-loss surgery and whether it should be removed preventively. Here’s what you need to know.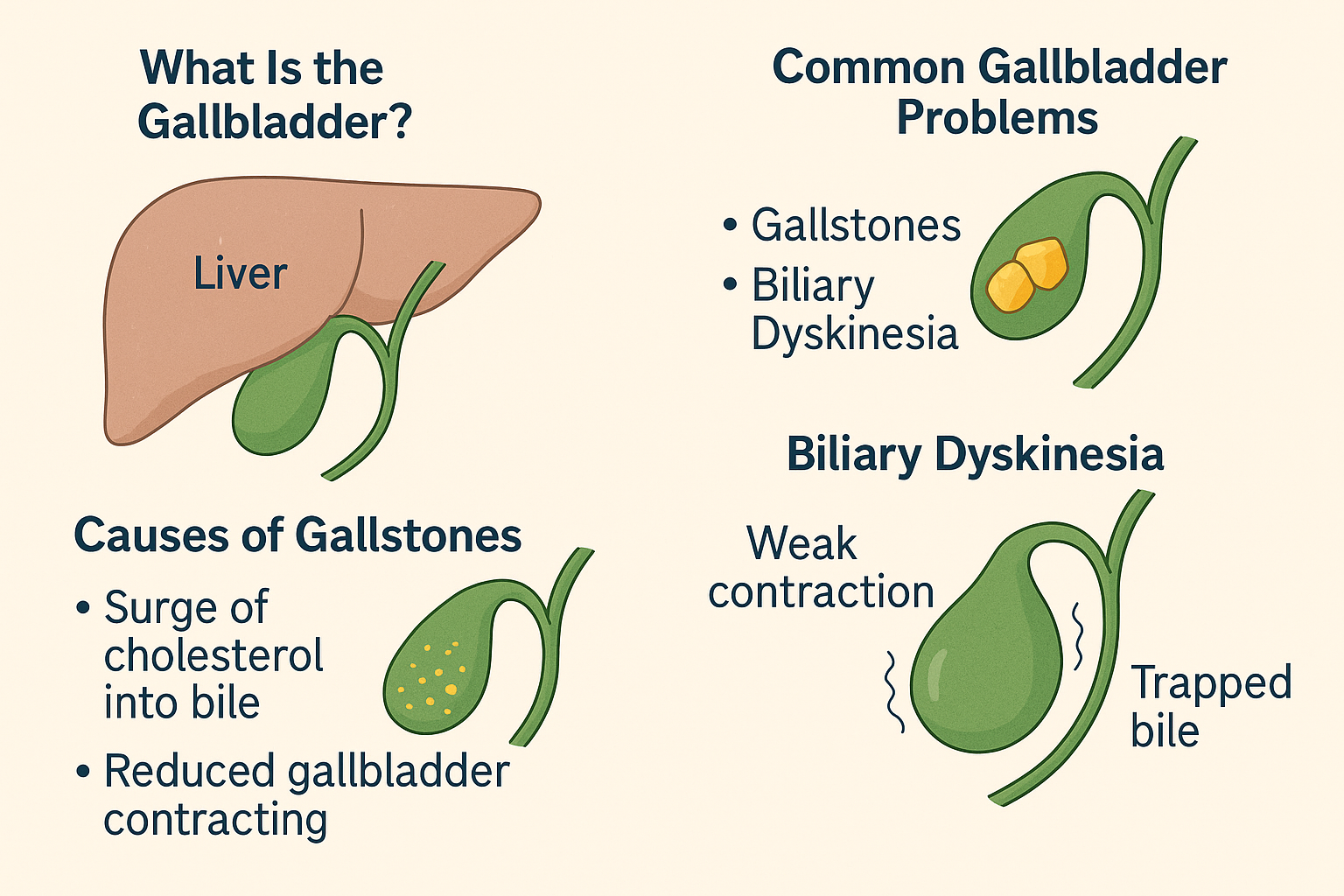
When Is Gallbladder Removal Necessary?
If gallbladder disease develops after bariatric surgery, the most effective and definitive treatment is surgical removal of the gallbladder, also known as a cholecystectomy.
Unlike kidney stones, gallstones cannot be dissolved or broken up with lithotripsy. Once symptoms occur, medical therapy is not successful, and surgery becomes the recommended treatment.
Why Prompt Treatment Matters
Untreated gallbladder disease can lead to significant and painful complications, including:
-
Severe abdominal pain
-
Nausea or vomiting
-
Infection of the gallbladder or liver
-
Pancreatitis (the most serious complication)
The longer inflammation continues, the more scarring develops—making surgery more difficult and recovery slower. Early treatment prevents these risks.
What to Expect During a Cholecystectomy
For most bariatric patients, a cholecystectomy is a straightforward outpatient procedure. Patients typically go home the same day.
At Texas Center for Bariatrics and Advanced Surgery, we use ultra–minimally invasive techniques with the da Vinci robotic surgical platform. This allows us to often:
-
Use the same small incisions from previous bariatric surgery
-
Reduce post-operative pain
-
Shorten recovery time
-
Improve surgical precision and outcomes
During surgery, the gallbladder is separated from the liver, the cystic duct is sealed and divided, and the gallbladder is removed through a tiny incision.
Recovery After Gallbladder Removal
Most patients recover quickly and return to normal activities shortly after surgery. Tips for healing include:
-
Avoiding fatty or heavy foods for 1–2 weeks
-
Limiting strenuous activity and heavy lifting briefly
-
Returning to work when comfortable, often within days
The majority of patients transition smoothly because the body adapts well to digesting fats without a gallbladder.
Should the Gallbladder Be Removed During Bariatric Surgery?
Some patients ask if their gallbladder should be removed at the same time as bariatric surgery to prevent issues later.
A preventive (prophylactic) cholecystectomy is only recommended if there is:
-
A history of gallbladder disease
-
Evidence of symptomatic gallstones prior to surgery
If the gallbladder is healthy and asymptomatic, removing it unnecessarily increases surgical risk and recovery time without benefit.
How to Prevent Gallstones After Bariatric Surgery
The best proven strategy to prevent gallstones after weight-loss surgery is Ursodiol, a medication that reduces gallstone formation.
-
We typically prescribe the brand Reltone.
-
It is taken for the first six months after bariatric surgery.
-
It reduces the risk of gallstones by 60–70%.
Without prevention, up to 40% of bariatric patients may develop gallstones within months. With Ursodiol, that number drops to about 2%.
How Ursodiol Works
Ursodiol helps protect the gallbladder by:
-
Lowering cholesterol in the bile
-
Increasing bile flow and cholesterol solubility
-
Improving gallbladder motility
This combination prevents the conditions that allow gallstones to form.
The medication has been used safely since the 1980s and is very well tolerated. Mild GI upset can occur, but most patients have no side effects.
Takeaway: Protecting Gut Health After Bariatric Surgery
Gallbladder issues can be a common side effect of rapid weight loss after bariatric surgery, but the good news is, they are preventable and treatable.
-
Ursodiol significantly lowers the risk of gallstones.
-
Robotic-assisted cholecystectomy is safe, routine, and effective when needed.
-
Proactive monitoring ensures early intervention and better outcomes.



